2003
Is Not Going To Be a Good Year
for Doctors
By David Gibson, MD
Introduction
Beginning
in January 2003, physicians in private practice will begin to experience a
precipitous drop in their office cash flow. They will see an explosive
increase in their accounts receivables and they will witness an uncontrollable
accumulation of uncollectible debt.
It
is now universally recognized that the “wheels are coming off the wagon” for
America’s employer based underwriting system for health care.
Seventy-five percent of all U.S. adults under age 65 get their health insurance
through the workplace. The LA Times
recently editorialized that “the growth in health-care premiums and in the
numbers of people without insurance represents an economic drag that business
cannot long endure and a level of unnecessary suffering a civilized nation
cannot in good conscience allow.”
Employers,
stunned by double-digit increases in health insurance premiums, are desperate
for cost-stabilizing alternatives. Here is the political reality that is
emerging. If the high deductible indemnity products, described in this
article, that are now being embraced by employers do not stabilize cost trends,
employers will simply no longer support the current private health care
underwriting system. The combination of a business/labor coalition coupled
with the usual entitlement expanding choir (the American Association of Retired
Persons and the Democratic Party) will represent an unstoppable political
tsunami that will produce a national single payer system similar to Medicare.
Health
care cost trends
Clearly,
health-care costs have taken a dramatic turn for the worse during the past five
years, rising more than 50 percent, with no end in sight. As a result, employers
consider this unrelenting rise their most serious business problem and they are
responding.
Large
employers have been stunned by a twelve-fold health-care premium increase in the
last decade. These companies
will spend an average 15 percent more on the cost of health coverage for
employees next year, according to a study recently released by Hewitt
Associates. The cost of health
insurance for large employers will increase 15.4 percent in 2003, compared to a
13.7 percent rise this year. Health insurance premium rates for HMOs will
increase 16 percent, and those for preferred provider organizations will
increase 15 percent, the study found.
Forty-six
million Americans work for small employers. These individuals typically
have less access to coverage than those in large firms. California small
to medium sized employers generate over half of all jobs. They have been
receiving premium increases for 2003 that run up to 60 percent.
Where
is the market going?
During
the last price spiral in late 1980s, employers turned to managed care, but the
latest round of health inflation has exposed the folly of its claims to control
costs. There is now a growing momentum away from “first dollar
coverage” managed care plans. HMO enrollment shrank by 640,000 this past
year with the trend accelerating into this year and beyond. In fact, other
than government employees covered under union bargaining agreements, no insurer,
other than Kaiser, is selling new HMO accounts in California today.
As
a result, managed care is both consolidating and imploding. All of the
regional health maintenance organizations (Omni, Health Plan of the Redwoods and
Lifeguard) have exited the market. By the end of 2002, California will
have 17 HMOs writing commercial policies, down from 21 in March.
Employers
are embracing indemnity products with high deductibles in an effort to align
inflationary rates for health care benefits with wages. Deductible limits
for PPO products increased 37 percent in 2001 according to the data published by
the Kaiser Family Foundation. Market data indicates that the deductible
has been increasing exponentially during this year and beyond.
To
monitor the dynamic movement of the health underwriting market, one must visit
with the employers who make payroll each month and the brokers who work directly
with them. Over the past several weeks, I have had the opportunity to
engage many of these individuals in informative conversation. The
following summarizes the profound restructuring of the health care underwriting
system they indicate is now well underway here in California and across the
nation.
The
dominant product now being embraced by the small to medium sized employer market
is high deductible ($1,000 per year with a $2,000+ out of pocket beyond the
deductible) catastrophic health insurance. The policy covers hospital
services only. Office visits are not covered. In patient
professional fees are covered at 20percent of the negotiated fee after the
deductible. There is no pharmacy benefit.
Employers
can choose to purchase “wrap products” that will enhance the catastrophic
product’s coverage. These wraps limit their liability for drugs and or
ambulatory professional services typically at $500 per year per beneficiary.
The
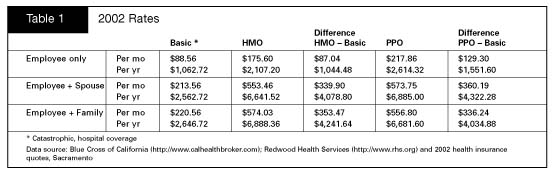
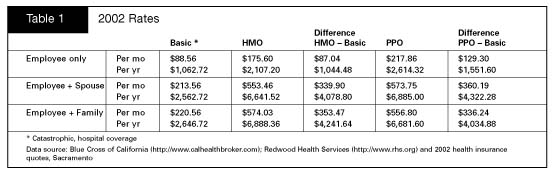
following table summarizes how this indemnity catastrophic coverage product
compares with existing managed care products this year.
The
just completed legislative session here in Sacramento produced a string of
successes for the Democratic Party's core constituent groups. As a result,
California’s employers are facing significant increases in their costs for
doing business. Governor Davis has signed legislation that mandates
increases in workman’s compensation, altered existing labor law and enriched
family leave benefits.
All
insurance costs from liability to fire and casualty have increased. Now
employers face continued significant increases in health benefits. The
differential per year between the catastrophic or basic product described above
and the HMO product is a $1 thousand per employee and $4.2 thousand per-family.
For PPO products the differential is $1.5 thousand and $4 thousand respectively.
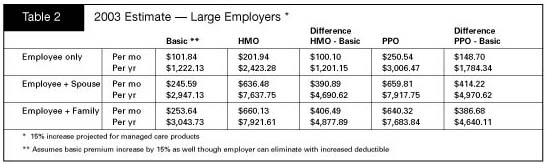
The
cost differentials for 2003 that are now being quoted to large employers are
summarized as follows:
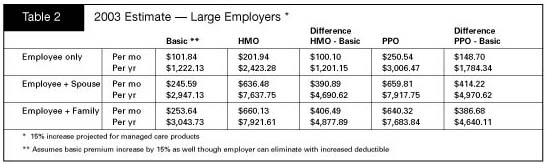
Large
employers are facing 15percent trends in their health premiums. This
produces annual cost differentials for the HMO vs. the catastrophic product of
$1.2 thousand for the individual and $4.8 thousand for the family. The
differential for the PPO product is $1.78 thousand and $4.64 thousand
respectively. It should be noted that the employer can avoid premium trends
beyond the general inflation rate for the catastrophic product by adjusting
upward the deductible limit.
The
following table demonstrates the reason for the rapid movement to catastrophic
by the small to medium employer market. These employers are facing
60percent increases in their group health premium costs for 2003.
Thus,
the small to mid sized employer that generates over half of all jobs in
California faces a cost differential next year between the catastrophic and the
HMO product of $2.15 thousand for the employee and $7.97 thousand for family
coverage. The differential for the PPO product is $2.96 thousand and $7.65
thousand respectively.
Physicians
are small employers. Their options next year are rather limited.
They can either drop coverage for their employees or absorb the increases
summarized above. The option of moving to a catastrophic product will be
hard to resist.
Uwe
Reinhardt, PhD, professor of health economics, Princeton University, sees an
evolving trend whereby employers, health insurers and the government are all
intent on pushing more health care costs onto consumers, a situation he expects
could create an enormous backlash against doctors and hospitals over the next
two to three years.
The
implications of a high deductible indemnity insurance product on the
physician’s practice
The
high deductible indemnity products that are now cannibalizing the market during
the current open enrollment season for 2003 coverage will have profound effects
upon the physician’s practice. Unless the altered business fundamentals
these new products bring to the market are factored into the physicians business
planning for next year, the physician will likely experience significant
reductions in cash flow, run-away accounts receivables that will never be
collected and an inability to meet business obligations.
If
you now have a significant portion of your revenue generated by capitation
contract; then prepare in advance for a substantial cash flow reductions. The
following cautionary tale is illustrative. At the time of writing this
article, the San Jose/Good
Samaritan Medical Group, the largest doctors' group in the South Bay, has just
announced bankruptcy.
The
San Jose Medical Group, founded in 1955, is a cornerstone of Silicon Valley
health care, at one point serving more than 170,000 patients. In recent years,
it has faced mounting financial problems due in part to declining reimbursements
from health insurers and the federal government. Those problems were exacerbated
by a sharp decline in the clinic’s capitated HMO patients, from 90,000 in 2001
to 60,000 in 2002.
Going
into a capitation contract is profitable. An individual physician or
medical group enjoys increased cash flow resulting from first of the month
capitation checks along with residuals from their previously developed accounts
receivables.
Coming
out of a capitation contract is another matter. Cash flow is immediately
reduced when the capitation checks stop and it takes 60 to 90 days to receive
payment from accumulated accounts receivables. This reality is at the core
of the San Jose Medical Group’s
bankruptcy.
Carefully
evaluate the liability associated with your network (IPA) contracts. Network
contracts, the staple of managed care, do not translate well into the high
deductible indemnity market. You may have many more of these contracts
than you realize. There is a vigorous secondary market where these
contracts are bought and sold on the national market. These contracts
dictate that the physician can only collect co-payment funds from the patient
after the claim has been adjudicated by the insurance administrator.
Unless the employer has purchased a wrap product, the catastrophic policy
contains no liability for professional services in the ambulatory setting.
Thus
the physician is bound by contract to provide service but can not collect until
the carrier confirms non-coverage. The likelihood of the physician
collecting from the patient will significantly decay after a 60 to 90 day
adjudication cycle.
Payment
at the time of service or arrangements for payment over time is an absolute
requirement for financial survival in the coming business environment for
physicians. Continuing to perform services under your existing IPA
contracts will only guarantee an out-of-control accounts receivable and
ultimately insolvency for the physician’s practice.
Invest
in your front office staff. You will need someone who can provide financial assistance to your
patients as they receive your unexpected bills for professional services.
This front office financial assistant must be able to set-up payment
arrangements for patients lacking the funds to pay for the services they
receive. The very survival of your practice depends upon the interpersonal
and financial skills of this individual.
Develop
a close business relationship with your bank. Physicians should not be in the business of consumer debt financing.
Work with the bank to have them rate debt, assume these consumer debt
liabilities and manage the collection process.
Conclusion
The
"managed care'' revolution in the 1990s transformed health care delivery by
imposing a leaner, meaner approach to business. Tough economic times now
threaten the most financially fragile health care businesses which include most
physicians’ practices.
Physicians are both health care professionals and small business men & women. The very fundamentals of the business of medicine will change dramatically beginning in January, 2003. To not recognize this reality is to invite insolvency for both individual and group practices in the immediate future.
© David J. Gibson, MD 2002